Note: I’m experimenting with Substack’s audio features. This week you can read the newsletter below, or listen to me read it by clicking the link above. Thanks!
“No amount of real resources devoted to medical research would have helped European society in 1348 to solve the riddle of the Black Death.” - Joel Mokyr (1998)
There is no currently existing human vaccine for covid-19. Can we force one into existence by promising to spend a lot on it? Is there some price at which we can “buy” a covid-19 vaccine in the next year?
That’s the premise of a proposal by economists Susan Athey, Michael Kremer, Christopher Snyder, and Alex Tabarrok. They propose the US government commit in advance to paying a substantial price for a specified number of vaccine doses: something like $100 each for the first 300 million. The idea is that the potential of winning $30bn will induce pharma companies to pour resources into vaccine development.
Covid-19 and the Profit Motive
We have lots of reasons to believe that a promise to pay more for a covid-19 vaccine would induce more covid-19 vaccine work. Academic research is moving so fast these days that we already have good evidence that pharma companies are extremely responsive to profit signals around covid-19. Bryan, Lemus, and Marshall (2020) track the number of covid-19 therapies at any stage of development, as well as the number of academic publications related to covid-19, to produce this stunning figure:

The black line that is shooting off to the top of the chart is the total number of therapies or publications related to covid-19, as measured against the number of days since the beginning of the pandemic/epidemic. The various dashed lines correspond to the number of therapies and publications for other diseases and/or pandemics (Ebola, Zika, H1N1, and breast cancer). Two things are immediately apparent.
First, covid-19 research is much higher than research related to other pandemic diseases. Second, the gap between covid-19 and other diseases has widened as the magnitude of the covid-19 pandemic becomes clearer. It seems obvious these differences are entirely driven by the difference in demand for a covid-19 therapy, both relative to other drugs and over time, rather than some scientific breakthrough that made it suddenly easier to do covid-19 research. So the above figure is strong evidence that pharma companies respond to profit opportunities and would probably respond further if the government promised to buy a working vaccine at a higher price than the market would normally support.
But dig into the data a bit deeper and there is something troubling. While a vaccine would be the most useful therapy, an unusually large share of the therapies under development are drugs, rather than vaccines. And while it would be nice if an existing drug turned out to be a useful therapy for covid-19, it seems more likely a new disease will require a new kind of drug. But repurposed drugs, rather than novel therapies account for an unusually large share of trials.
This difference has grown over time, as the scope of the pandemic widened. And the divergence between vaccines vs. drugs, and novel drugs vs. repurposed ones, is significantly larger for covid-19 than for Ebola, Zika, and H1N1.

This suggests the rising profitability of a covid-19 treatment is pushing ever more firms to focus on therapies that are not necessarily the best treatment for the disease, but which are most likely to get to the market soon. Vaccines tend to be harder than drugs, and novel drugs tend to be harder than repurposing existing drugs.
It turns out the above evidence is quite consistent with existing research on how medical research responds to market demand. We have good evidence that government promises to pay more for vaccines would likely induce more vaccine research. But the evidence we have also suggests such a policy is most effective at bringing to market a vaccine that does not require much more R&D (but read the ending of this newsletter for caveats).
Markets for Vaccines
The kind of program Athey, Kremer, Snyder, and Tabarrok are proposing is called an Advance Market Commitment, and it’s been successfully tried before. In 2007, a coalition of governments and the Gates Foundation pledged $1.5bn towards the production of 200 million annual doses of a pneumococcal conjugate vaccine for developing countries. If a manufacturer would supply the vaccine at a price of no more than $3.50 per dose, the advance market commitment would top up the rest with a share of the $1.5bn pledged. The program launched in 2009 and in 2010 GSK and Pfizer each committed to supply 30 million doses annually. This amount was increased over time, and a third supplier entered in 2019. Annual distribution exceeded 160 million doses annually by 2016.
Uptake of the pneumococcus vaccine was much faster than uptake for vaccines for a different virus without an advance market commitment (rotavirus). So the advance market commitment seems to have worked.

But there's an important caveat to all this: very little R&D was required to develop the pneumococcal conjugate vaccine. When it was selected, vaccines for similar diseases in developed countries already existed, and vaccines covering the strains in developing countries were already in late-stage clinical trials. So in this case, the advance market commitment pushed firms to quickly build up manufacturing and distribution capacity, but it didn’t push them to do extensive R&D since none was needed.
This is the only time a large-scale advance market commitment has been tried. But that’s not the only place we can look for evidence.
Finkelstein (2004) identifies three US policy changes that increased the profitability of vaccines for some diseases but not others. She then looks to see if firms respond by creating more new vaccines for the affected diseases, relative to the unaffected diseases. Indeed, they do. Let's dig in a bit more.
The three policies Finkelstein uses are (1) the 1991 CDC recommendation that all infants be vaccinated against Hepatitis B; (2) the 1993 decision for Medicare to fully cover the cost of influenza vaccination for Medicare recipients and; (3) the 1986 creation of the Vaccine Injury Compensation Fund which indemnified vaccine manufacturers from lawsuits relating to adverse effects for some specified vaccines. In each of these three cases, policy choices made vaccines for some diseases more profitable, but had no effect on other diseases.
As a control group, Finkelstein considers various sets of alternative diseases that were not affected by these policies, but which otherwise share some of the same characteristics as the affected diseases. All told, she has data on preclinical trials, clinical trials, and vaccine approvals for 6 affected diseases and control groups consisting of 7-26 other diseases, over 1983-1999.
Diseases where policy increased profitability saw an additional 1.2 clinical trials per year and an additional 0.3 new approved vaccines per year (but only 7 years after the policy took effect), as compared to controls. So the promise of more profit did pull in more vaccine development.
But the effect only travels so far up the research stream. When Finkelstein looks farther up the development pipeline, the effect disappears. Affected diseases had no more preclinical trials than the control group. This suggests firms responded to the increased profit by pulling vaccines already far along off the shelf and putting them into clinical trials. But if it stimulated more basic research, the effect was too small to be detected.
Markets for Drugs
There is also a rich vein of research on the extent to which general pharma R&D (not vaccines) respond to changes in the size of the market for different health products. Dubois, Mouson, Scott-Morton, and Seabright (2015) look at the link between potential profits and innovation in the context of global pharmaceutical innovation. They've got a data on drug sales in 14 major countries, which they use to make estimates of the size of the market for different categories of therapeutic medicine. Their goal is to see how changes in the size of the market for a drug change the propensity to develop new drugs for the market. In this case, they're holding the measure of innovation to a relatively high bar: a newly approved drug, marketed in one of their 14 countries, that is also a new chemical entity (i.e., not a modification of an existing drug).
One challenge is that better drugs can, themselves, change the size of the market. Suppose for example, that new drugs just come along randomly as a result of serendipity. In that case, potential profit doesn't actually induce firms to develop new drugs. But if these new drugs find a market, and we're measuring the size of the market by looking at spending on drugs, then we'll create a misleading correlation between the "size" of the market and the number of new drugs. In this case, the number of drugs is "causing" the size of the market, rather than vice-versa. To avoid this, they use a statistical technique (instrumental variables) to pull out the parts of demand that vary due to demographics and overall GDP growth (neither of which should be affected by drug innovation over the 11-year period they work with).
When they do this, they find that bigger markets do indeed lead to more drugs. On average, when the market for a therapeutic category grows by 10%, there are 2.6% more new chemical entities approved over a given time period.
But how scientifically novel are these new drugs? Suggestive evidence comes from Acemoglu and Linn (2004), who perform a similar exercise as Dubois, Mouson, Scott-Morton and Seabright (2015), but on US rather than global sales data. When the market for different diseases in the US changes due to shifting demographics, how does this change the flow of new drug approvals for those diseases? Acemoglu and Linn find the effect of a bigger market is much, much stronger for generic drugs than for new molecular entities.
More direct evidence comes from Dranove, Garthwaite, and Hermosilla (2020) who also investigates this question in the context of global drug development over 1997-2018. They use the US Medicare Part D extension to see if the promise of higher profits leads led firms to pursue more scientifically novel drugs.
The basic idea is that Medicare Part D extended medicare to pay for enrollee's pharmaceutical drugs beginning in 2006. This created a big new market for drugs used by Medicare enrollees (US residents aged 65 and up). Dranove, Garthwaite, and Hermosilla have data on worldwide pharmaceutical company drug trials, and they want to see if companies run more trials on scientifically novel drugs in response to the new opportunities created by Medicare part D.
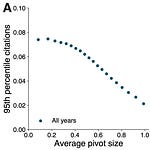
To measure the scientific novelty of a drug, Dranove, Garthwaite, and Hermosilla count the number of times the specific "target-based action" of the drug has been explored in previous drug trials (of similar or stronger intensity). A target based action comprises the specific (targeted) biological entity and the mechanism used to modify its function: for example, a p38 MAP kinase inhibitor is a target-based action that targets the p38 mitogen-activated protein kinases and inhibits its function. If this target-based action has never before been used in a clinical trial, then a drug using it is considered maximally novel. The more often it has been previously used, the less novel.
With this measure in hand and data on 76,161 clinical trials on 36,002 molecules, Dranove, Garthwaite, and Hermosilla look to see if therapeutic areas with greater profit potential in the wake of Medicare Part D see more clinical trials for scientifically novel drugs. While they do find that more exposed therapeutic areas do see a small increase in trials for the most novel kinds of drugs, once again the effect is much stronger for the least novel drugs. Over 2012-2018 the number of trials for the least novel group of drugs increased 106%, while the number of trials for the most novel group increased just 14% (with most of the gains coming in the second half of that period).

Can We Buy a Covid-19 Vaccine?
So back to covid-19. Can an advance market commitment “buy” a vaccine that doesn’t yet exist? Or are we in the same position as Joel Mokyr’s medieval kings, whose wealth can’t buy any treatment for the bubonic plague until someone thinks of the germ theory of diseases?
First, the studies above suggest these policies do work, but are most effective if the vaccine does not require too much more R&D. Does a covid-19 vaccine require a lot more research? I don’t know. On the one hand, there hasn’t been a human vaccine for this class of virus before. On the other hand, there have been vaccines for veterinary applications (innovation in human and animal health has a lot of similarities), and there seems to be no shortage of options.
Second, the size of the proposed policy is enormous relative to what’s been tried before. So even if these policies normally only work weakly on vaccines that are far from approval, it may be that we still observe a large effect simply because we’re pouring so much money into it.
Third, one of the goals of the Athey, Kremer, Snyder, Tabarrok proposal is explicitly to build manufacturing capacity for vaccines before they are proven, so that we can mass produce them as soon as we find one that works. To the extent building capacity is not a problem that requires R&D, than advance market commitments should work very well. In general, an advance market commitment is only one (albeit big) part of a set of complementary incentives the authors recommend to push and pull a vaccine to market. Give the whole thing a read!








Share this post